
If you’re looking for sciatica treatment, this post will walk you through practical options—when to see a doctor, common tests, treatment choices, rehab, and how to return to sport safely.
First, an important point: sciatica isn’t really a single “disease name.” It’s a symptom label for leg pain or numbness that travels from the lower back through the buttock and down the leg, usually because a nerve is irritated somewhere along its pathway.
The causes vary. Common ones include lumbar disc herniation and lumbar spinal stenosis, where the nerve root is compressed or irritated in the lower back.
Bottom line: good sciatica treatment starts with identifying the likely cause and combining pain-smart movement with step-by-step rehab. Many people improve over time—but some cases linger, so don’t ignore red flags.
• Common causes of sciatica and why the pain travels
• Simple self-checks (including red flags and when to seek care)
• Medical tests (MRI, etc.) and treatment options (conservative care, injections, surgery)
• How to progress rehab, typical timelines, and tips to reduce recurrence
• FAQs
目次
- 1 What is sciatica? (Definition)
- 2 Causes of sciatica (What triggers symptoms?)
- 3 Symptoms (Common complaints)
- 4 Self-checks (when to see a doctor)
- 5 Medical tests for sciatica (MRI and more)
- 6 Treatment (conservative care, injections, surgery)
- 7 Sciatica rehabilitation
- 8 Expected timeline (How long does it take to recover?)
- 9 FAQ
- 10 Summary
- 11 References
What is sciatica? (Definition)
Sciatica refers to radiating pain (pain that spreads down the leg) and/or numbness that follows the nerve pathway from the low back toward the leg (see Fig. 1).
It often happens on one side, and in some cases you may notice weakness (for example, difficulty lifting the toes) in addition to pain [3].
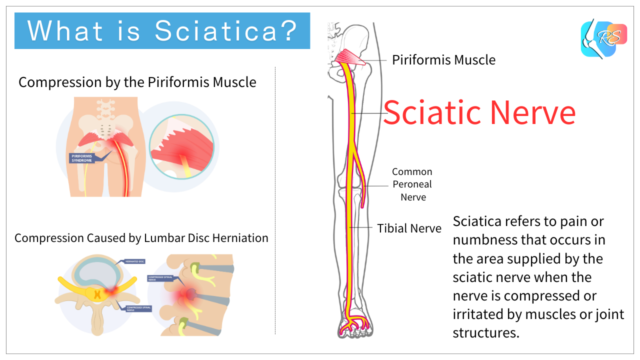

Think of “sciatica” as a symptom name. For example, if a lumbar disc herniation is the cause, it’s more accurate to think in terms of “sciatica due to a lumbar disc herniation.” Identifying the cause helps guide the right plan [3].
Causes of sciatica (What triggers symptoms?)
There are several possible causes, but the most common is nerve root compression from a lumbar disc herniation. Other causes include lumbar spinal stenosis, and more rarely, tumors or other serious conditions [3].
Sometimes the irritation happens outside the spine, such as piriformis syndrome, where the nerve is irritated deep in the buttock. The key point is that different causes need different strategies.
When sciatica symptoms often worsen (Aggravating factors)
These situations commonly make symptoms worse (though they aren’t always the “root cause”):
- Prolonged sitting (car rides, desk work, classes)
- Repeated bending forward (lifting, washing your face, putting on socks)
- Heavy weight training (especially with poor form or excessive load)
- Sudden sprints, kicking, or jumping in sports (be extra careful during painful phases)

Symptoms (Common complaints)
• Symptoms may worsen with prolonged sitting and may change with standing or walking
• Hip flexion + knee extension can reproduce symptoms (often during a straight-leg raise test)
• In severe cases: weakness (e.g., difficulty lifting the toes) or reduced sensation
The typical pattern is pain or numbness that follows the nerve down the leg—often from the buttock into the back of the thigh, then into the calf or foot.
Self-checks (when to see a doctor)
Top priority: “red flags” that warrant prompt evaluation
• Trouble urinating or having bowel movements, inability to pass urine, or incontinence
• Numbness in the groin/saddle area
• Worsening weakness in the leg (sudden change in walking, foot drop, etc.)
• Fever, history of cancer, or severe constant pain at rest
Quick checks (pain pattern and reproduction)
- Pain/numbness often travels below the knee (calf to foot)
- Coughing, sneezing, or straining can sometimes increase leg symptoms
- Symptoms may be reproduced with a straight-leg raise (SLR) or slump test (Fig. 2)
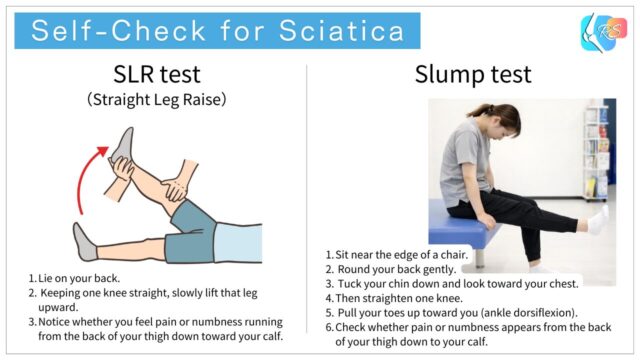
Just keep in mind: self-checks can’t confirm the exact cause on their own.
If your pain is severe, keeps lasting, or numbness is getting worse, it’s safer to get a proper evaluation.
Medical tests for sciatica (MRI and more)
To evaluate sciatica, clinicians combine history and physical examination (including a neurological exam) with imaging when needed [3].
- MRI: helpful for assessing disc herniation, nerve compression, and stenosis
- X-ray: checks spinal alignment and bony changes (often used as part of narrowing down the cause)
- Neurological findings: strength, sensation, reflexes, and tests like SLR to assess nerve involvement
Treatment (conservative care, injections, surgery)
Conservative care (the usual first step)
For most people, the first approach is conservative treatment (non-surgical care) [3].
This often combines physiotherapy (exercise + movement coaching) with medication and other strategies to control symptoms and help you return to daily life and sport [1].
Injections (e.g., epidural steroid injections)
If pain is severe, clinicians may consider options such as epidural corticosteroid injections. A review suggests they may offer small, short-term pain relief compared with placebo, while uncertainties remain regarding overall benefits and safety [4].
Surgery (when is it considered?)
Surgery may be considered when there is progressive neurological deficit (such as worsening weakness) or when symptoms do not improve with adequate conservative care [3].
For example, in persistent sciatica from lumbar disc herniation (around 4–12 months), one trial reported that microdiscectomy improved pain at 6 months compared with non-surgical care [5].
Whether to stay conservative or consider injections/surgery depends on severity, duration, and whether weakness is present. Always decide together with your clinician [3].
Sciatica rehabilitation
Now let’s go through key rehab ideas for conservative management.
The main goals are: controlling nerve-related pain, improving hip and pelvic movement, and building better trunk stability.
• Make sure pain and numbness are not getting worse.

Try to organize your daily life so nerve pain doesn’t flare up. Little adjustments in posture and activity can make a big difference.
• Practice breathing strategies (e.g., abdominal pressure control)
• Gentle stretching/massage for buttock, thigh, lower leg, and foot—stop immediately if symptoms flare
• Train other areas safely as long as it doesn’t trigger symptoms

• Strength training for glutes, hips, thighs, and trunk
• Once symptom-free strengthening has started, gradually begin easy jogging after ~1–2 weeks
• Slowly increase straight-line running speed
Watch out for flare-ups—this is a common timing for symptoms to return if you progress too fast.
• Begin sport-specific movements (be careful with kicking motions if that tends to flare symptoms)
• Add reaction drills and partner-based drills as appropriate
• Keep stretching as a maintenance habit
Expected timeline (How long does it take to recover?)
Recovery speed varies from person to person. Many improve over time, but research suggests that a certain proportion still have symptoms at 12 months [2].
Longer symptom duration and certain beliefs (such as “I think this will last a long time”) have been associated with a slower recovery in some reports [2]. When pain is intense, anxiety often rises—so getting evaluated early and having a clear plan can really help.
FAQ
Q1. Can stretching cure sciatica?
Stretching can help some people, but the right approach depends on whether the main issue is nerve root compression in the spine or irritation around the buttock area. Aggressive stretching can make symptoms worse, so if pain or numbness is strong, it’s safer to get evaluated [3].
Q2. Do I always need an MRI?
Not necessarily. But MRI is often considered when symptoms are severe, persistent, associated with weakness, or when red flags are present [3].
Q3. Do epidural steroid injections work?
Reviews suggest they may provide small, short-term relief compared with placebo. Whether they’re appropriate depends on your situation, so discuss this with your clinician [4].
Q4. Are there cases where surgery is necessary?
Surgery may be considered if neurological deficits worsen (like progressive weakness) or if symptoms don’t improve despite adequate conservative care [3]. In persistent disc-herniation-related sciatica, surgery improved pain at 6 months in one study [5].
Q5. Can I keep playing sports?
When symptoms are strong, many sport-specific movements can aggravate pain, so you often need temporary modification (rest, reduced volume/intensity). The goal is a gradual return while monitoring symptoms closely [1].
Summary
Sciatica is a symptom pattern—radiating pain or numbness from the low back toward the leg. Common causes include lumbar disc herniation and lumbar spinal stenosis.
Many cases improve with conservative care, but some last longer. If you have red flags (bowel/bladder problems, saddle numbness, worsening weakness, etc.), seek medical care promptly.
Rehab focuses on symptom control, improving movement (including hips and trunk), and gradually rebuilding training loads so you can return to sport without flare-ups.
References




